Lowering the cost of prescription drugs is a perennial priority. Pharmacists are in a position to help patients manage chronic illness and medication use, which can greatly reduce spending.
By Jane E. Rooney
Given the country’s aging population and the increasing prevalence of chronic diseases, healthcare spending isn’t likely to decrease anytime soon. With the presidential election only a year away, it’s also guaranteed to be a topic that receives plenty of attention. The Centers for Medicare & Medicaid Services reported that U.S. healthcare spending increased 3.9 percent to reach $3.5 trillion, or $10,739 per person, in 2017.
Healthcare spending growth in 2017 was similar to average growth from 2008 to 2013, which preceded the faster growth experienced during the 2014-15 period that was marked by insurance coverage expansion and high rates of growth in retail prescription drug spending. A CNBC report from 2017 indicated that experts predict spending per person will reach $14,944 in 2023. Prescription drug spending, which accounted for almost one in every 10 dollars spent on healthcare in 2013, saw spending growth on account of a number of blockbuster drugs getting generic competition in 2012.
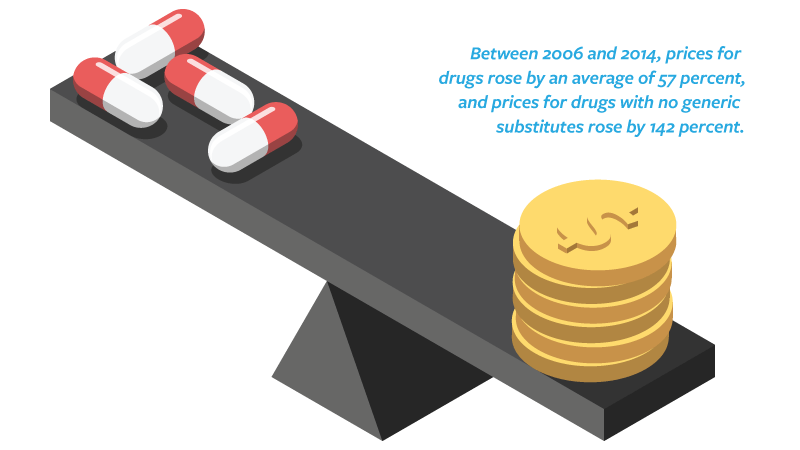
A 2018 Washington Post article explains why drug prices have gotten so high: “In 2006, prescription drug coverage became part of Medicare, introducing a massive influx of patients with prescription drug coverage into the market. Pharmacy benefit managers (PBMs) took on an additional role for a wide range of health plans: helping plans set formularies (the terms on which patients can access drugs) and negotiating prices with drug companies. The rise in prices that followed has been dramatic. Between 2006 and 2014, prices for drugs rose by an average of 57 percent, and prices for drugs with no generic substitutes rose by 142 percent.”
The issue of drug pricing is central to the debate about how to control healthcare spending. U.S. Department of Health and Human Services Secretary Alex Azar identified drug pricing as one of four main priorities for the agency. The goal is to lower the cost of prescription drugs for all Americans and to boost transparency around price and quality.