The healthcare community has reached consensus, but has a conundrum: ‘We need CMM, but how do we do it?’
By Athena Ponushis
Patients benefit from comprehensive medication management (CMM). Physicians benefit from CMM. Pharmacists no longer have to sell the need for CMM, now they just need to figure out how to implement it and sustain it. That comes from a consistent approach.
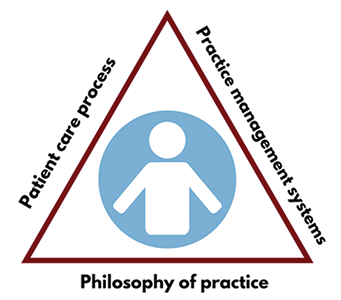
“A consistent approach to the patient care process for CMM is essential if we’re going to ensure that what we’re doing is effective, can be scaled and can be sustained,” said Dr. Mary Roth McClurg, professor and executive vice dean at the at the University of North Carolina at Chapel Hill Eshelman School of Pharmacy and the principal investigator of a rigorous study to assess the implementation and effectiveness of CMM in primary care practices.
Advancing the role of pharmacists in primary care, and advancing CMM to further the safe and effective use of medications, starts with a common language, clear intentions and consistent delivery. Schools of pharmacy are eager to put CMM into practice, and that enthusiasm was evident at the Concordia Medication Management Accelerator (CMMA) live pitch event at Concordia University Wisconsin (CUW) in November, where speeding up implementation took on a “Shark Tank” vibe.
Accelerating CMM
A personal donation of $250,000 to the CUW School of Pharmacy from Mr. Erv Dohmen was allocated for the school to do something to advance pharmacy practice in Wisconsin. Dr. Andy Traynor, chair and associate professor of pharmacy practice at Concordia, said such a broad directive got administrators thinking, “What creative things are going on around us? Where are areas of need? Where are opportunities that align with how we feel we are preparing our students to serve their communities?”
This train of thought led Concordia to the Alliance for Integrated Medication Management (AIMM), a national nonprofit known for its work with health systems, primary care clinics and community pharmacists to drive change in the delivery of care. Collaborating with AIMM and connecting with Concordia’s Batterman School of Business, Traynor said he and his colleagues started thinking, “What if we took AIMM-style coaching and processes, and the entrepreneurial experience of our business school, to our students and our local healthcare practices? We could really move the needle on advancing CMM.”
CMMA was born. Fifty-five attendees from 27 different organizations across the state came to the launch. The urgency and deep-down reason for CMM was reemphasized: better care, better outcomes, lower costs. Teams were assembled. Two tracks were laid out: the service accelerator, for established organizations looking to advance or adopt CMM within their practice, and the start-up accelerator, for businesses or innovators who had an idea that would provide a CMM service.
Teams looked to their communities and organizations to identify populations of focus and needs. Using a process known as the Business Model Canvas, teams spent five months outlining their ideas and testing them where their ideas were weak, so they could hone their work and give a solid, final pitch. They were coached over the phone, in person and online.
Then came the “Shark Tank” moment: the live pitch. Team members gave 10-minute pitches in front of four expert, CMM-savvy judges, competing for more than $60,000 in awards. Pitches were passionate, pharmacists were supported and the commitment to CMM was clear, showcasing a need to continue the charge.
“Schools need to strive for further innovation at that interface of community engagement, practice and science, and I think we also need to go into that realizing that we can’t do it on our own,” Traynor said. “There are great experts and perspectives outside our schools of pharmacy who we can collaborate with to work on these things. The work of our practice community, not just our faculty, needs to be a focus.”