A Novel Approach to Pharmacy Instruction
By Jane E. Rooney
Schools of pharmacy are incorporating the arts and humanities into the curriculum to give students more insight into patients’ experiences, foster greater empathy and strengthen the patient-provider connection.
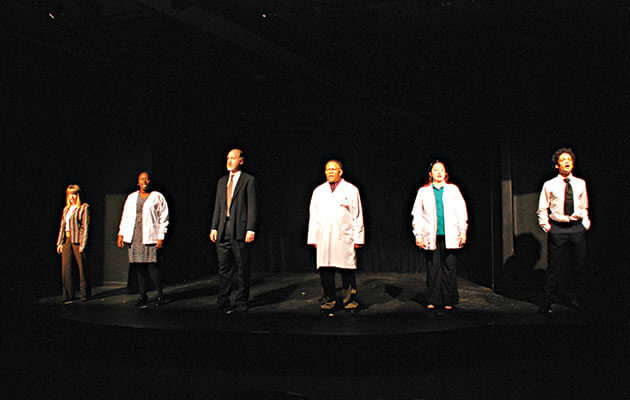
A student pharmacist can open a textbook and get a straightforward, technically accurate explanation of a disease or medication. But what if that student read a piece of literature that offered a vivid description of someone suffering from illness? Or saw a play in which an actor portrayed what it looks like to live with a certain disease? Or had to create a dance based on a medication’s chemical structure? The arts and humanities are making their way into classroom instruction at several pharmacy schools as faculty attempt to broaden students’ understanding of the patient experience and ultimately enhance the patient-provider relationship.
“The humanities are able to provide a much better depiction and scope of what people actually experience when they are ill,” explained Dr. Russell Teagarden, former VP of clinical practices and therapeutics at Medco Health Solutions. “The humanities give a fuller explanation as it relates to the prolonged illness experience. It lets students and practitioners get a better grasp of the fullness of that experience. The way that writers, artists, musicians, filmmakers and poets are able to render it in a very profound way makes a much bigger impact. It’s much more powerful and an entirely different experience of reading about an illness in literature rather than in a textbook.”
Along with faculty at Touro College of Pharmacy, Teagarden received AACP’s Innovations in Teaching Award in 2011 for developing an elective course, “Illness Performed and Imagined,” that explored how healthcare is interpreted and portrayed across several humanities genres, including literature, art, film and drama. The intent, Teagarden said, was to expose students to the humanities as a place to get a broader view of illness and expand the scope of inquiry they would have with any given disease. “We purposely used different genres to show students that getting a better picture of an illness can be found in a lot of different places. If you have a fuller understanding of what people face, you’d hope that would trigger empathy but also that you would ensure that treatment and diagnoses are better.” This approach also reinforces the idea behind narrative medicine: helping providers understand a patient’s whole story.
Courses like these, along with visual arts displays and other performance experiences, are engaging student pharmacists and allowing them to gain a deeper understanding of how patients live with illness, how medication impacts their lives and why more empathic interactions with their healthcare providers can make a difference. “I’ve come to see the arts as essential to producing good clinicians,” Teagarden declared. “I don’t think it’s just nice to have, I think it’s critical to put it into the curriculum.”